Let's Talk About Obesity
We've got the doctor-approved details on obesity causes, symptoms, treatments, and a jillion other facts and tips for living with the condition.
Living with obesityisn’t always easy; besides the health complications you may be experiencing, our society places an enormous stigma on individuals who are overweight. You may feel embarrassed or ashamed. But we at HealthCentral are here to tell you that you shouldn't have to feel that way. For starters, you’re not alone—far from it. Millions of other people living with this condition feel or have felt just like you do right now. We—and they—are here for you. On this page alone, you’ll discover the realities and challenges of obesity, along with the best treatments, helpful lifestyle changes, and all the crucial information to help you not just manage—but thrive. We’re sure you’ve got a lot of questions...and we’re here to answer them.
Our Pro Panel
We went to some of the nation's top experts on obesity to bring you the most up-to-date information possible.

Angela Fitch, M.D.
Associate Director of the Massachusetts General Hospital Weight Center, Vice President of the Obesity Medicine Association
Boston, MA

Sara N. Bleich, Ph.D.
Professor of Public Health Policy
Harvard Chan School of Public Health
Boston, MA

John Kirwan, Ph.D.
Executive Director
Louisiana State University's Pennington Biomedical Research Center
Baton Rouge, LA
没有单一的、孤立的因素决定whether a person will develop obesity. Rather, it’s caused by a complex interplay of biological, psychological, and environmental triggers—everything from calorie consumption and genetics to socioeconomics and medications a person takes. Despite the way obesity is often portrayed, it is not caused by a lack of willpower.
Get your calculator ready. Obesity is defined using a relatively simple mathematical equation:Weight (in kilograms) / Height (in meters) squared = Body Mass Index. Most doctors consider an adult Body Mass Index, or BMI, of 30 or more to be obese. In words, obesity can be defined as a diagnosable medical condition that occurs when an individual’s body accumulates and stores excess amounts of body fat.
Obesity is the second leading cause of preventable death in the U.S. According to a recent study published in the我nternational Journal of Obesity, people who have obesity live 5.6 to 7.6 fewer years than their healthy-weight counterparts.
From a BMI POV, someone who is overweight has BMI of 25.0 to 29.9, while a person with a BMI of 30 or more is considered to have obesity. Both conditions have the potential to pave the way towards similar health concerns.
What Is Obesity, Anyway?
First, let’s talk about what obesityisn’t. It’s not a character flaw, a sign of laziness, or evidence of a lack of control. It’s not a reason to feel shamed or be made the punch line of a joke. Just liketype 1 diabetesormultiple sclerosis, obesity is a disease—and a difficult-to-control one, at that.
我t’s a legitimate medical condition that occurs when your body accumulates and stores excess amounts of fat. Depending on one’s height and weight, obesity is divided into several categories, including Class 1, Class 2, and Class 3.
Class 3 is sometimes referred to as“severe” or “extreme” obesity. (The term “morbid obesity” is now considered archaic and overly stigmatizing. Translation: Don’t use it to describe yourself or others.)
与普遍认为,人们不选择to develop obesity; most people don’t wake up one morning and think, “Hey, today is a good day to become overweight to the point where it might damage my health and well-being.” Obesity is a result of a complex back-and-forth interplay of biological, psychological, and environmental triggers.
Yes, nutrition and exercise matter, but with every passing year, researchers are uncovering more and more possible contributing factors, from lack of sleep to various popular medications to gut bacteria, and even childhood ear infections.
And while society as a whole seems to have no problem poking fun at those with obesity via memes and jokes, the truth is that obesity is now the norm in our country. According to new research published in theNew England Journal of Medicine, 40% of the U.S. population is currently living with obesity and that number is projected to rise to nearly half of the American population by the year 2030. Contributing to eight of the 10 leading causes of death in the U.S., obesity is a public health epidemic—and there's nothing funny about that.

What Causes Obesity in the First Place?
At its most basic level, obesity is a result of an imbalance in caloric intake and expenditure: When you consume more calories than you burn through exercise and activities of daily living, you create what is called a “positive energy balance”—your body has taken in more fuel than it can use. If that continues unchecked, it can lead to weight gain and, possibly, obesity.
But there’s far more to this challenging condition than just, “Whoops, I ate too many fries.” Nor can obesity be blamed entirely on genetics, as has often been the case.
Experts now believe that environment—the social, economic, cultural, and even physical factors that surround us every day—hold enormous sway over what we eat, how much we consume, and how quickly or inefficiently we burn it off.
Here are some of the most common culprits believed to be behind the obesity epidemic:
An Obesogenic Environment
Experts think a constellation of environmental factors may be responsible, in part, for prompting us to eat more calories in a day than needed. Together, they create what is called an obesogenic, or obesity-promoting, environment. Some of these features include:
A shift towards snacking. Those calories tend to be in addition to our meals, meaning we don’t compensate for that 3 p.m. bag of chips by eating less at dinner.
Mushrooming portion sizes. A typical fast food beverage in the 1950s was seven ounces. Today's drinks are often 42 ounces. Meanwhile, hamburgers and fry portions have tripled in size.
Widespread availability of ultra-processed foods. We’re talking candy, cookies, chips, and soda—all of which somehow manage to be calorically high yet nutritionally devoid.
Drifting away from home cooking. More than half of our calories come from outside the home. These dishes tend to be higher in fat and sugar than home-cooked food.
Targeted marketing. If you shop online for a certain less-than-healthy snack, targeted ads for similar products will start popping up on your social media feed. In another form of targeted marketing, companies that make fast food, soda, and other processed foods are known to concentrate their marketing efforts in black and Hispanic communities.
Access to cars and public transportation. Driving everywhere means there’s no need to walk, and walking burns calories. Less calorie-burn while eating the same amount of food raises the odds of weight gain.
Calorie Quality
Not all calories are created equal. What we mean by that is that 100 calories of almonds don’t affect your weight in the same way as 100 calories of nachos. Your body has to work harder to digest foods that are rich in fiber and protein than it does to digest refined carbohydrates, such as white bread, pasta, and candy. Researchers call this the “thermic effect” of food.
我n a study published in theAmerican Journal of Clinical Nutrition, subjects ate the same diet with the same number of calories for six weeks with one exception: when it came to grains, one group incorporated whole grains (brown rice, whole wheat bread, and oats) while the other ate refined grains like white bread. Those people in the whole grain group burned nearly 100 more calories per day, simply due to thermic effect.
Genetics
According to the Obesity Medicine Association, genetics increase the odds of obesity by anywhere from 40% to 70%, and there are more than 200 genes known to be strongly associated with the disease. If these genes are not working properly, it's important to understand that while they raise the risk of developing obesity, they by no means guarantee it. For the vast majority of people, when it comes to your weight, your fate is truly in your hands. Genes may also interact with the environment to increase or decrease one’s odds of gaining an unhealthy amount of weight.
Medications
A laundry list of prescription medications have been linked with weight gain, including steroids, antidepressants, hormonal contraceptives, medications for diabetes, bipolar disorder, insomnia, high blood pressure, seizures, epilepsy, and more.
Sleep
A humming metabolism and well-balanced hunger hormones are among the bevy of health-promoting effects that happen when we log enough Zzzzs. Proper sleep helps balance the hormones that make us feel hungry or full (ghrelin and leptin, respectively).
Too little sleep and ghrelin soars, driving you to eat more. Not to mention, staying up later gives you more time to eat, which also contributes to weight gain. In the landmark Nurses’ Health Study, which followed 68,000 middle-age American women for up to 16 years, women who slept for five hours or less were 15% more likely to develop obesity compared with those who slept seven hours a night.
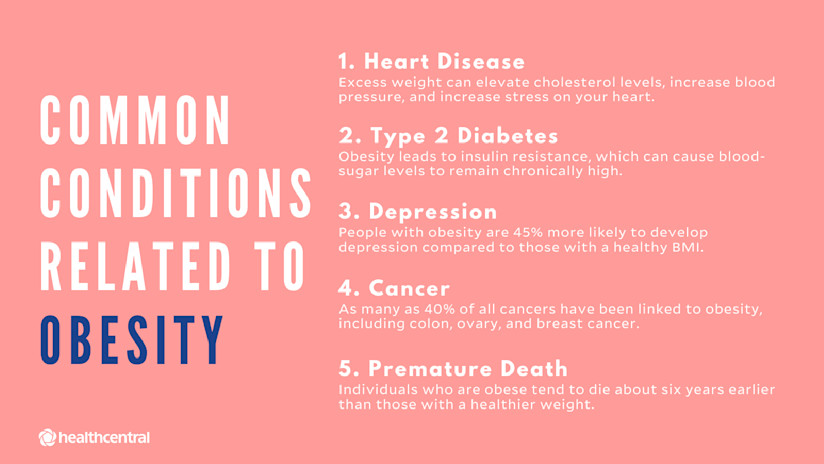
Does Obesity Put Me at Risk for Other Conditions?
Obesity rarely occurs in a bubble. While some people may be obese and have no serious co-existing medical conditions, they are the exception. As the second leading cause of preventable death in the U.S.,obesity is a serious public health concern with far-reaching implicationsand reams of studies have linked it with more than 200 chronic diseases. Here are a few:
Heart Disease
随身携带多余的体重可以把pressure on the heart, forcing it to work harder to send blood throughout the body. Individuals who are overweight or have obesity also tend to have conditions that independently raise the risk forheart disease, such as elevated cholesterol and high blood pressure.
Type 2 Diabetes
我n this increasingly common condition, a person’s blood sugar levels become chronically elevated. Up to 90% of adults withtype 2 diabetescarry extra weight or have obesity, perhaps because excess weight causes cells to become more resistant to a hormone called insulin, which is responsible for ferrying sugar from blood to muscle and fat cells, where it can be used for energy. With insulin resistance, sugar remains in the blood for an inappropriate amount of time, creating inflammation. Complications of high blood sugar include heart disease, stroke, kidney disease, amputation, and blindness.
Depression
The psychological impact of obesity may contribute todepression, especially in women. In an Australian study, researchers compared the data of more than 48,000 people with depression with data of nearly 300,000 without it. They found that individuals who had obesity were 45% more likely to develop depression compared with those who had a healthy Body Mass Index. (Body Mass Index is defined as a person’s weight in kilograms divided by the square of their height in meters.) The link may be due to genetic variations, the social stigma of carrying extra weight, or other factors.
Cancer
Up to a staggering 40% of allcancersare linked to obesity. Doctors have found connections between obesity and these cancers:
Breast(specifically, in post-menopausal women)
Gall bladder
Liver
Pancreas
Thyroid
Cancer happens when cells in a part of the body grow abnormally or in an out-of-control manner. We don’t know exactly why obesity—or even just carrying extra weight—seems to drive cancer rates, but one theory is that fat cells may release hormones that impact this abnormal cell growth. Poor eating habits and/or a lack of physical activity also fuels cancer risk.
Premature Death
According to a recent study published in the我nternational Journal of Obesity, people who have obesity live 5.6 to 7.6 fewer years than healthy-weight people. Those who have severe obesity can expect to live 8.1 to 10.3 years less.
…And More
Sleep disturbances and acid reflux, along with low back pain, arthritis, and other complications caused by excessive stress being placed on the bones and joints, are also caused by obesity.
How Do Doctors Diagnose Obesity?
我n 2013, the American Medical Association officially recognized obesity as a disease. This was a huge step forward in the eyes of many doctors and patients, as it served as an announcement to the nation that obesity is not a personal choice, but a complex, legitimate health condition.
认识到肥胖作为一种疾病也很重要because it means that, like cancer, Crohn’s disease, and other widely-accepted medical conditions, health care providers can write prescriptions for treatment.
How to Calculate BMI
When diagnosing, most doctors and medical organizations use a measure called Body Mass Index (BMI) to determine whether a person has obesity or not. BMI is calculated via the following mathematic equation (Warning: You’ll likely need to use anonline conversion tool, as it utilizes the international system of units):
Weight (in kilograms) / Height (in meters) squared = BMI
For adults…
BMI of 25.0 to 29.9 = overweight
BMI of 30 or more = obese
To put that in perspective, a woman who is 5’4” and weighs 175 is considered obese (BMI of 30). The same goes for a 5’9” man who weighs 204 pounds (BMI of 30.3).
Obesity is further divided by class:
Class 1 = BMI of 30.0 to 34.9
Class 2 = BMI of 35.0 to 39.9
Class 3, or severe obesity = BMI ≥40.0
Arguments exist both for and against using BMI as a diagnostic tool. Those in favor of using it appreciate the fact that it’s a fast, easy, no-cost calculation, and say it offers a quick but reliable snapshot of a person’s risk.
Opponents feel it may be a misleading measurement, either incorrectly categorizing some people having obesity, as it doesn’t take muscle mass or body frame into account (in athletic individuals or those with highly muscular builds, for instance) or, more dangerously, classifying some people as healthy simply because they have a "normal" BMI, when in fact they may be at risk for weight-related health conditions due towherethey carry their fat.
People who carry their weight around the belly ("apple" body types), for instance, are at increased risk for cardiovascular disease over those who carry more weight around their hips ("pear" type), even if they have a medically acceptable BMI. Belly fat is more worrisome when it comes to the effects of obesity.
Some believe that a more progressive diagnostic tool would account for not just excess body fat, but the presence of adverse health effects caused by that body fat (see above).
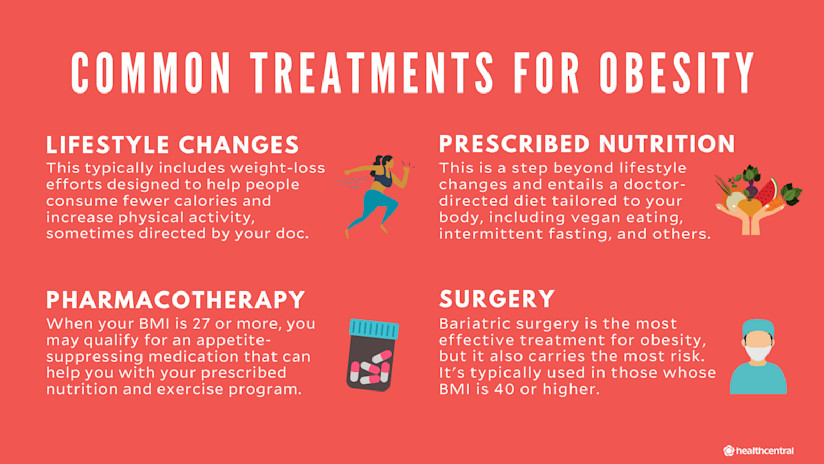
What Are the Best Treatments for Obesity?
我f you think obesity seems like a complicated disease, its treatments are equally complex. Physiologically speaking, it’s difficult to lose a significant amount of weight and keep it off. “Eat less and move more” is great advice when you have 10 pounds to shed; less so when you need to unload 50 or more. (In fact, while exercise is vital for weight maintenance, research suggests it's less effective in helping people to lose large amounts, unless you're work out at a super-intense level.)
So yes, the struggle is real. Ready for some encouraging news? Losing just 3% to 5% of your weight—and maintaining that loss—has the power to bring about important improvements in health. You can stabilize your blood sugar levels, lower your risk of developing type 2 diabetes, and more. Dropping more than that helps improve heart health and may be enough to reduce the dose of medication you take for various related chronic diseases.
考虑到这一点,check out the obesity treatment strategiesexperts currently employ to help people fight obesity, and their odds of success.
Lifestyle Modification
This category typically includes weight loss efforts designed to help people consume fewer calories and increase physical activity. If you’re working with a healthcare provider, she or he may recommend adding behavior change tools to help you stay on track, such as setting specific, attainable goals; keeping a food and exercise journal; and digging deep to learn about the environmental cues that prompt you to eat in unhealthy ways.
Percent of people who will reach their weight-loss goal using lifestyle modifications: 2% to 5%
Prescriptive Nutritional Interventions
A step beyond lifestyle medication, this category involves specific, prescribed behavioral modifications tailored to the individual’s unique environmental and genetic risk factors, with the goal of creating some sort of weight-loss advantage. Possibilities include (but are not limited to):
vegetarian or vegan eating
therapeutic carbohydrate reduction (a.k.a. the Keto diet)
Percent of people who will reach their weight-loss goal using prescriptive nutritional interventions: 5% to 10%
Pharmacotherapy
The Food and Drug Administration has approved several medications for weight loss and chronic weight management. You need a BMI greater than 30 to qualify for a prescription, though those with a BMI greater than 27 as well as a weight-related health complication are eligible as well, even though they’re not technically obese.
A few examples of medications include:
Alli (Orlistat)- This drug works by blocking the absorption of dietary fat. When taken, about 30% less fat is absorbed from food and eliminated in the stool.
Ozempic (Semaglutide)- Already used to treat diabetes, this drug is expected to be available for obesity by 2021. It belongs to a class of drugs called GLP-1 receptor agonists, and studies suggest it can help some people lose as much as 20% of their weight.
Suprenza (Phentermine)- This stimulant targets neurotransmitters in the brain that dampen appetite.
Pharmacotherapy requires medical supervision and is used in combination with nutrition and lifestyle changes.
Percent of people who will reach their weight-loss goal using pharmacotherapy: 5% to 20%
Endoscopic Procedures
The term “endoscopic” means a doctor uses a tiny, flexible instrument to enter your gut through your mouth. Once inside, one of a number of approaches may be used to help reduce food intake. These include anintragastric balloon, which is exactly what it sounds like: a balloon is inflated in the stomach, where it takes up space to lower your appetite and encourage the patient to consume smaller portions. Inendoscopic suturing, tiny stitches are sewn into the inside of the stomach, making a person feel fuller on less food.
在upside, endoscopic procedures are done on a same-day, outpatient basis, and are less invasive than surgery (meaning fewer risks). On the downside, they are not yet covered by insurance, so you can expect to pay $5,000 to $8,000 out of pocket.
Percent of people who will reach their weight-loss goal using these endoscopic methods: 10% to 20%
Metabolic Surgery (a.k.a. bariatric surgery)
This is the treatment category with the most risk but also greatest success rate. Surgery is usually reserved for people with a BMI higher than 40, or a BMI over 35 along with an obesity-related health condition. It has the potential to not just drastically reduce your weight, but to also help manage, improve or even reverse more than 40 obesity-related conditions, including heart disease, sleep apnea, high cholesterol, certain cancers, and more. In some trials, 70% of patients who undergo surgery show remission of type 2 diabetes within a few days.
A few types of metabolic surgery include:
胃旁路手术- A surgeon essentially creates a new, much smaller stomach, then connects it directly to the small intestine. The first step reduces the amount of food that can be comfortably consumed (about two to six ounces at a time), and the second step prevents the body from absorbing as many calories as it otherwise would.
Gastric Sleeve (a.k.a. Vertical Sleeve Gastrectomy)- Like gastric bypass, this limits how much a person can eat. Unlike gastric bypass, about 80% of the stomach is removed. “The Sleeve” also has a strong effect on appetite-regulating hormones, so people generally just feel less hungry after the procedure.
我nsurance companies typicallydocover metabolic surgery, so long as you meet the proper criteria.
Percent of people who will reach their weight-loss goal using bariatric surgical methods: 20% to 40%
What’s Life Like for People with Obesity?
我ndividuals affected by excess weight and obesity are on the receiving end of unwarranted disapproval and shaming by others in the workplace, in the dating world, at their doctor’s office, when dining out, at the gym, or just at the corner store, as other customers assess and judge their purchases. Studies have concluded that weight stigma is as pervasive as racial stigma.
The effects of being treated as unworthy of respect or love can be emotionally haunting and physically and psychologically dangerous. Poor self-esteem, depression, and even suicidal thoughts have all been widely reported in individuals affected by obesity.
Weight bias also impacts how and whether a person chooses to access health care. For example, studies have shown that women with obesity tend to skip preventive care appointments and routine gynecologic cancer screenings. Reasons include wanting to avoid interacting with providers who had previously expressed a negative attitude towards their weight or given unsolicited weight loss advice; fearing being asked to wear a too-small gown or sit on a too-small examining table; not wanting to be weighed; you get the point. The result is a supremely unhelpful catch-22, causing those who need medical help the most to avoid it.
我ronically, some of the more successful forms of treatment, such as surgery, are themselves stigmatized. No one would ever fault a woman with breast cancer for needing a mastectomy, yet that’s a common response to hearing of someone electing to undergo metabolic surgery. (“Wow, what a failure. She couldn’t lose it on her own.”)
Still, society is slowly moving forward with an understanding that obesity is a disease and not a lifestyle choice. Using respectful language (“person with obesity” instead of “obese person”) is a major step in the right direction, and exciting work is being done with regards to public health policy and treatment innovation.
我f you are living with obesity, finding a multidisciplinary weight loss team (they’re often affiliated with a university) can help you come up with a strategy to take control of your health. Through one of these teams, you’ll have access to physicians, psychologists, nutritionists, exercise specialists, and other experts who want to help you, judgement-free.
Where Can I Find My Obesity Communities?
Power in numbers, right? With 40% of Americans currently living with obesity, this community has no shortage of people who are right there with you. This community finds a way to encourage each other —willeach other — into a healthier future. Being a part of this world may seem daunting right now, but these influencers and orgs will help you come to terms with the number on the scale, and through their own journeys, encourage you to start your own.
Top Obesity-Related Instagrammers
Stella,@stellaisstriving
Follow because:她开始在567磅,她已经失去了超过43%f that weight. No surgery, just food changes and exercise. No miracle drug, just pure determination. Does she have setbacks? Of course—she’s human. But she keeps pushing, and she shares every pound lost, every sweat of morsel shed, and every encouraging word on her feed, daily.
Shannon Taylor,@shannons_story
Follow because:Like most people who set off on a weight-loss journey, Shannon’s did not stick the first time around... or even the fifth. It wasn’t until he met his medical match — his gastric sleeve surgeon — that it finally clicked. He’s the epitome of the saying, if it doesn’t work the first time, try, try again. He’s now on the road to completing an Ironman, but will never forget where he came from, so he shares the inspiration for how he got from there, to here, on his feed.
Nichole,@pretty.n.sleeved
Follow because:There is NO shame in her sleeve game. One of the best quotes on her feed could not ring more true: “Weight-loss surgery is NOT the easy way out because the surgery only works if YOU do.” Having weight-loss surgery still has its own host of hardships, and it’s not for everyone. She squashes the stigma of surgery being the scapegoat from obesity, while constantly reigniting her self-accountability to keep going.
Mike "Gormy” Gorman,@gormy_goes_keto
Follow because:He’s not going to sugarcoat it. It’s hard work and tough choices, every single day. But for someone who ate his way down (yes, ate his way down) from 540lbs to 205lbs, he’ll tell you it’s worth it. Gormy shares his keto lifestyle, while also spilling some life lessons about living with obesity—including the mental “weight” on your shoulders that comes along with this condition.
Top Obesity-Related Podcasts
The Fat Guy Forum.Gormy’s back again — and this time with a podcast that not only chronicles his 300lb weight loss, but also shines the spotlight on other men with phenomenal weight loss journeys. They come from all walks of life and hearing their tactics from each POV will suck you in for hours (or days...).
Obesity Panacea Podcast.Two Ph.D. candidates with a fascination for obesity and weight-loss host this podcast, which feature reviews on new products, promising programs, and trends for weight-loss. They bring in the experts to dive into options for obesity, but also the mental and social norms around this disease.
This Podcast Burns Fat.我n case the name of the podcast wasn’t telling enough... this podcast aims to help you eat clean, find the workouts that are right for you, and ultimately, burn fat. Backed by hosts Dr. Lori Shemek, and health coach Omar Cumberbatch, this is the podcast you listen to when you need the knowledge about getting healthyandthe encouraging daily push.
Top Obesity-Related Orgs and Support Groups
The Obesity Society.This nonprofit organization believes there’s a science behind obesity — it’s not just about your environment and life choices, it’s chemical, it’s inside you. While helping you understand that, they also do the work to create science-based treatments to change your life.
Obesity Action Coalition.Need a provider for your obesity journey? They got you. Feeling like it would be best to be in a community for this process? They have one. Want to attend face-to-face or virtual conference to keep you reinvigorated? Come on down. This nonprofit has everything you need to actually be successful on your weight-loss journey.
LEAD for Rare Obesity.This incredible group supports those with genetic disorders of obesity, like POMC, LEPR, PWS, and others that you likely only know if you are affected by one of them. Being a part of this group (and there aremanysupport groups to choose from within LEAD) makes you feel like — maybe for the first time in your life — that you’re understood.
- Adolescents Sleep and Obesity:Massachusetts General Hospital. (2019). “Importance of when adolescents sleep to obesity and cardiometabolic health.”sciencedaily.com/releases/2019/09/190916110604.htm
- Gut Bacteria and Obesity:Lund University. (2018). “New link between gut bacteria and obesity.”sciencedaily.com/releases/2018/02/180223092441.htm
- Obesity and Childhood Ear Infections:American Psychological Association. (n.d.)“A surprising link to obesity.”apa.org/monitor/2008/10/ear-infection
- Obesity Prediction:Harvard. (2019). “Close to half of U.S. population projected to have obesity by 2030.”news.harvard.edu/gazette/story/2019/12/close-to-half-of-u-s-population-projected-to-have-obesity-by-2030/
- Obesity Epidemic:Pharmaconomics. (2015). “The Epidemiology of Obesity: A Big Picture.”ncbi.nlm.nih.gov/pmc/articles/PMC4859313/
- 我mpact of Whole Grains:The American Journal of Clinical Nutrition. (2017). “ Substituting whole grains for refined grains in a 6-wk randomized trial favorably affects energy-balance metrics in healthy men and postmenopausal women.”academic.oup.com/ajcn/article/105/3/589/4637849
- Primary Obesity:Journal of Translational Medicine. (2019). “Why primary obesity is a disease?”ncbi.nlm.nih.gov/pmc/articles/PMC6530037/
- 肥胖并发症:National Institute of Diabetes and Digestive and Kidney Diseases. “Health Risks of Being Overweight.”niddk.nih.gov/health-information/weight-management/health-risks-overweight#type2
- Obesity Clinical Issues:Endotext. (2018). “Clinical Problems Caused by Obesity.”ncbi.nlm.nih.gov/books/NBK278973/
- Diabetes and Bariatric Surgery:我nternational Journal of Environmental Research and Public Health. (2019). “Remission of Type 2 Diabetes Mellitus after Bariatric Surgery: Fact or Fiction?”ncbi.nlm.nih.gov/pmc/articles/PMC6747427/
- Stigma of Obesity:Journal for Nurse Practitioners. (2016). “Obesity Stigma and Bias.”ncbi.nlm.nih.gov/pmc/articles/PMC5386399/
- Obesity Epidemic and Stigma:BMC Medicine. (2018). “How and why weight stigma drives the obesity ‘epidemic’ and harms health.”bmcmedicine.biomedcentral.com/articles/10.1186/s12916-018-1116-5
- BMI, Depression, and Genetics:我nternational Journal of Epidemiology. (2018). “Using genetics to understand the causal influence of higher BMI on depression.”academic.oup.com/ije/article/48/3/834/5155677
- Depression Comorbidity:British Journal of General Practice. (2014). “Prevalence of comorbid depression and obesity in general practice: a cross-sectional survey.”bjgp.org/content/64/620/e122
- Obesity and Cancer:American College of Cardiology. (2016). “The Relationship Between Obesity and Cancer.”acc.org/latest-in-cardiology/articles/2016/10/06/10/05/the-relationship-between-obesity-and-cancer
- Obesity and Life Expectancy:我nternational Journal of Obesity. (2018). “Impact of Overweight, Obesity and Severe Obesity on Life Expectancy of Australian Adults.”ncbi.nlm.nih.gov/pubmed/30283076
- Cancer and Body Fat:New England Journal of Medicine. (2016). “Body Fatness and Cancer — Viewpoint of the IARC Working Group.”nejm.org/doi/10.1056/NEJMsr1606602
The Latest on Obesity

12 Tips to Stop Overeating During the Holidays (and Beyond)
Let's Talk About Obesity Medication

Let's Talk About Obesity Treatment


